Glocal health Consultants
"Glocal support on glocal issues –
health policy and implementation thought leadership"
A brief overview of Healthy Cities evidence
A long history of cities and health
The connection between health and urbanisation has been inescapable since early human settlement, or rather, when paleo-epidemiologists and archaeologists determined an evolution from hamlet and villages to cities. This first happened by the end of the Neolithic, some 10,000 years ago, in Mesopotamia and the Levant, a few thousand years later followed by great fortified cities in the Indus Valley. A next wave of urbanisation happened some 3000 years ago on the rim of the Mediterranean and Black Sea (Greek city states and Persian urban development). These early, often fairly isolated, cities and city-states have become the dominant form of human settlement in the 21st century: never before more humans have lived in cities. And some of these cities almost transcend human scale (e.g., Shanghai) and imagination (e.g., Qatar).
Health considerations have always been part of urban development. In the earliest Mesopotamian cities urban planners carefully left instructions for safe food storage, water supply, and sewage disposal. These traditions have not always continued on a steady upward evolutionary slope: medieval European cities were considered cesspools of human misery, not just for the poor. Infectious disease outbreaks were rampant throughout the centuries, driven by a toxic combination of urban parameters. Such city living can be characterised as follows:
- dense crowding of humans and other life forms (e.g., rats and fleas – causing the bubonic Black Death in the 14th century; but more recently SARS connected to poultry);
- trade and mobility (which led to medieval Venice to introduce one of the first state-led public health measures: quarantine); and
- the opportunity to enjoy and exploit human diversity (in human and social relations, but also in education and cultural development).
It is no wonder that the modern public health revolution of the 19th century came about as a consequence of rapid urbanisation. The cultural vanguard of the Enlightenment (e.g., Voltaire for Paris) had commented on the abysmal state of cities and how crowding and abject living conditions affected the quality of life of the masses. De Villermé applied emerging statistical analyses to produce a health demographic of French workers, and in the Anglosaxon world the birth of modern public health was heralded when John Snow first removed the handle of the Broad Street pump in response to his cholera incidence inquiry, and was subsequently instrumental, with Edwin Chadwick and an emerging middle class movement called the ‘Hygienists’, in advocating for public health legislation.
An epidemiological transition, and the birth of Healthy Cities
Public health historians have identified two epidemiological transitions:
- The Neolithic epidemiological transition from small relatively healthy communities to larger families (due to increased food security and more stable, settlement-based, opportunities for mother and child health) and from a range of causes of disease and death (most dominantly deliberate or accidental violence) to mostly zoonotic infectious disease (10,000-3,000 ago, and still with cascade effects in some parts of the world);
- The ‘modern’ epidemiological transition from infectious disease to chronic disease. Non-communicable disease is now considered, as reaffirmed at the level of the United Nations by government leaders’, as the one major health challenge of the 21st
Urban health in the 19th century – hygiene
Early precursors of ‘Healthy Cities’ (the 19th century Hausmann redesign of Paris; Ebenezer Howard’s call for the building of ‘Garden Cities’, and Dutch reformists like Wibaut and Querido driving the design of new Amsterdam suburbs specifically for labourers) addressed the concerns and circumstances of the times, notably those of infectious disease hygiene and working conditions. These ‘hardware’ approaches to healthy urban planning looked at the development of clean, uncluttered, airy, ‘visible’ infrastructure (e.g., wide boulevards), a manageable and interconnected ‘invisible’ infrastructure for water and sewage treatment (e.g., through managed underground sewage and transport systems), and opportunities for the masses to access green spaces for relaxation (e.g., Central Park in New York City, a project by Frederick Law Olmsted who was not just a landscape designer but vocal social critic).
Major social developments in the 20th and 21st century coincided with, impacted on, or were driven by, significant epidemiologic changes. The emphasis on worker health and infectious disease control, at least in the urban planning tradition, was replaced by a strong argument to include communities, values, systems and more ‘intangible’ resources (e.g., wellbeing) in the processes to plan, design and manage urban environments. Such arguments came about as a consequence of, among others:
- full suffrage (the right to vote and be elected) in ‘Western’ democracies since the late 1800s; the growth of a strong middle class;
- social justice and civil rights movements gaining momentum after the Second World War;
- a concern about environmental and planetary sustainability that gained credence since the Club of Rome reports (1972);
- the growth of global NGOs advocating for action globally and locally on health (Medecins Sans Frontieres), justice (Human Rights Watch and Amnesty International), governance (Transparency International), the environment (Greenpeace) etc.;
- certain political fads and faves, e.g., New Public Management (sometimes equated – wrongly – with Thatcherism, Reaganomics or neo-liberalism);
- a globalisation of goods (e.g., trade), beliefs (e.g., popular culture) and services (e.g., banking) helped by growing communications and IT services.
Connection urban health to social change and innovation
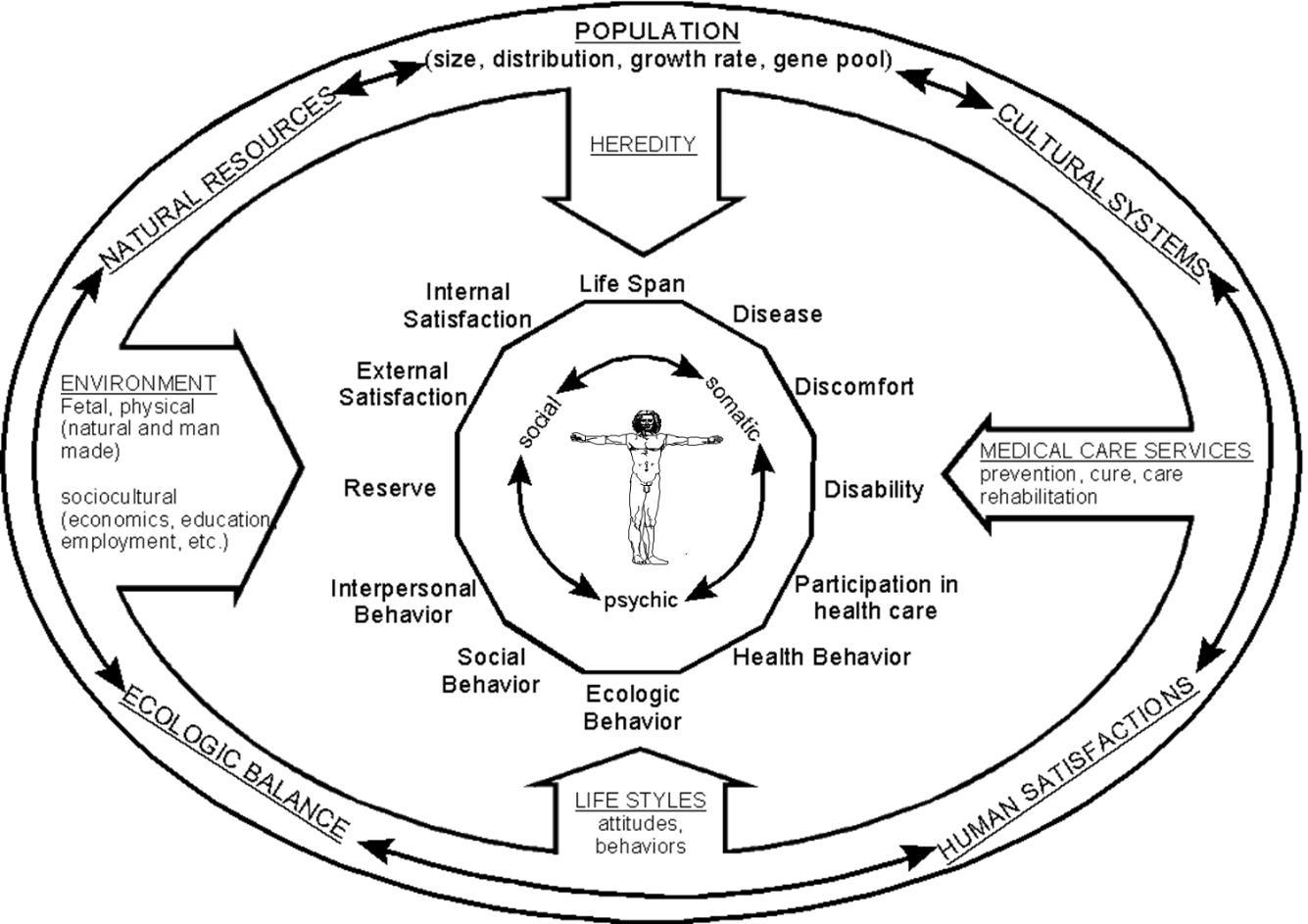
One of the first to recognise the interplay of these factors at the urban level was US psychiatrist Leonard Duhl who edited a 1963 book ‘The Urban Condition – People and Policy in the Metropolis’. His thinking connected with government initiatives that recognised broader determinants of health, e.g., the 1974 Lalonde Report from Canada. This report, in turn, relied heavily on early academic writings on the determinants of health, e.g., the Health Field Concept postulated by Henrik Blum (a friend and colleague of Duhl’s) in 1974.
WHO, in the midst of a reorientation that also involved the development of ‘a new public health’ (and adopted as the Ottawa Charter for Health Promotion in 1986), embraced the idea of ‘Healthy Cities’ as a formal programme deliverable.At a 1984 conference in Toronto, celebrating the anniversary of the Lalonde Report, Duhl and his Canadian colleague Trevor Hancock proposed that it would be possible to create a ‘Healthy City’. This idea resonated with European aspirations to formulate a strategy to attain Health for All by the Year 2000, driven by the European Regional Office of WHO but already adopted by some local governments, notably in Britain.
Healthy Cities as an idea, ambition, commitment, and programme
The launch of European Healthy Cities was supported by a series of booklets in which the evidence base and action areas were outlined. Hancock and Duhl authored the first one (‘Promoting Health in the Urban Context’) in which they reviewed the literature and determined eleven qualities a Healthy City should strive to provide.

As a working definition for the Healthy City they proposed (and found endorsement by WHO and the initial group of European cities) that it is a city:
…that is continually creating and improving those physical and social environments and expanding those community resources which enable people to mutually support each other in performing all the functions of life and in developing to their maximum potential.
Soon the European network of Healthy Cities started to expand, Australian and Canadian cities joined the global movement, and existing local and urban initiatives around the world (e.g., the Americas’ Healthy Communities efforts that were inspired by a strong commitment to local implementation of the Alma Ata Declaration’s vision of Primary Health Care through SILOS – Sistemas Integrales Locales para la Salud) adopted a ‘Healthy City’ rhetoric.
The many faces of a Healthy City
Through the World Health Organization
Since their ‘official’ launch in 1986 Healthy Cities have evolved and grown naturally and in great diversity. There has been general support for the initiative by WHO in its different regions, but this support has come in different shapes, directions, and times. The strongest effort seems to be made by the European Region where the Healthy City Movement has been working with cities and National Networks continuously over nearly thirty years. This has been facilitated by a sustained personnel presence in the WHO Office (with Dr. Agis Tsouros successfully championing and leading the various iterations of the programme) and an enthusiastic and committed network of city representatives and academic supporters. The European Healthy City approach is strictly codified, yet recognising the unique diversity between cities. The programme is urban government based, and requires formal designation through the submission of documentation on deliverables, processes and governance arrangements, endorsed by a formal political statement (usually a Council decision). One of the commitments each city expresses is to take action on the development of a national network of Healthy Cities. Designated Healthy Cities become a resource hub for other cities in a member state that want to work on the aspirations. WHO/EURO Healthy Cities work in Phases of approximately five years (thus transcending the ‘regular’ WHO budget cycle), in which strategic and thematic priorities need to be addressed. Currently the network operates in Phase VI. Each of the Phases has been evaluated – with increasing sophistication (below). The ‘unity in diversity’ approach in the designation process means that although all European Healthy Cities sign up to the same parameters and values, the operational aspects of their implementation can be wildly diverse. In a comparative evaluation of five UK and five Dutch Healthy Cities, Goumans (1998) found that Healthy Cities can be, and are being, driven and championed by many sectors, including education, social work, police, infrastructure and transport, parks and recreation, etc. In most but not all the health sector is represented.
Other WHO Regions have expressed commitments to the Healthy City idea, too. PAHO has consistently cherished and supported local government action for health (e.g., through resource packs for Mayors and other local politicians) but has not engaged in the formalisation of networking. WPRO has always had a number of member states where Healthy Cities were high on the agenda, initially with Australia and Japan, and Malaysia (Kuching) a consistent presence. Since the turn of the century the region has formally acknowledged the need to focus on urbanization and health, and guidance documentation and a strategic programme in this area have been developed. WPRO is not proactive in its approach of ‘designated’ cities – but through its networking efforts many cities across the region have signed up as a ‘Healthy City’ (e.g., in Cambodia, Mongolia, Laos, etc., with an abundance of cities in the Republic of Korea). However, there is no formal programme that establishes monitored relations between local governments and WPRO. EMRO has over the last five years revitalised a fledgling Healthy Cities and Villages programme, building on active programmes notably in the Gulf and Iran. Again, no formal designation, support or recognition has been developed. AFRO has always been active in Healthy Cities, and has been supported by a global Francophone network (Europe and Quebec) in growing capacities for Healthy Cities in its French speaking countries. After some initial initiatives in SEARO (e.g., Cox’s Bazaar, Bangla Desh) the Healthy Cities and urbanization argument seems to have disappeared from the Region’s agenda, although in some member states (notably Indonesia) many Healthy City-type efforts remain. Globally, after initial support from Headquarters, engaging in World Health Day 1996 (“Healthy Cities for a Better Life”) the emphasis shifted to the World Health Organization Kobe Centre (WKC) which has urban health as one of its official remits. WKC develops tools in collaboration with health authorities, e.g., the Urban HEART methodology (Urban Health Equity Assessment and Response Tool – Kumaresan et al., 2010) which is offered to (local) governments to identify and reduce health inequities at the city level. The tool has been applied widely, and is reported on in the peer-reviewed literature notably from Iran and the Philippines.
Through national government schemes
Of course local government does not need WHO support for the development and implementation of urban health activities. In fact, in many countries legislative schemes exist that have taken ideas of social determinants of health and Healthy Cities as an inspiration. The Republic of Korea is on such country, which has a proliferation of dozens of Healthy Cities, often associated with local civil society and academia (Nam et al., 2011) – there is an emerging evaluation and reporting tradition there that follows earlier surges in Japan (e.g., Takano, 2003). Another example is the Australian state of Victoria where a Public Health and Well-Being Act exists that is inspired by social determinants evidence, the Ottawa Charter, and Healthy Cities thinking (see ‘Case study: environments for health policy research – Environments for Health (E4H) policy effectiveness’ in De Leeuw, Clavier & Breton, 2014) – but the hundreds of Victorian municipalities that produce the required health plans do not identify themselves as Healthy Cities. Even more interestingly perhaps, Healthy Cities are not necessarily driven by, or accountable to, local government. Two of the longest-running Healthy Cities in the world (Kiama/Illawara in New South Wales, and Noarlunga/Onkaparinga in South Australia, both Australian states) are run by civil society foundations which may – or may not – connect to an official government health agenda.
This situation has been recognised by several international NGOs, the most active of which seems to be the Alliance for Healthy Cities with a membership of hundreds in Asia and Oceania. Although the Alliance keeps a repository of case studies and members’ health policies, and organises regular scientific conferences, there is a dearth of systematic and peer-reviewed evaluation output from this rich resource.
Healthy City evaluations
Since the mid-1980s there has been a proliferation of Healthy City initiatives around the world, with local governments and civil societies often adopting an eclectic mix of objectives and emphases. In some cases a comprehensive, value-driven and long term perspective is taken (by designated cities in the European Region of WHO, and some of the European National Networks). Such an approach lends itself to larger and more systematic evaluation efforts.
In other cases Healthy Cities have wanted to evidence the outcomes of their particular emphases, e.g., on oral health in Brazil (Moysés et al., 2006). But not all urban health interventions should be labelled as Healthy City initiatives – they should at the very least demonstrate an engagement with a broader social determinants of health discourse, recognise profound social and community involvement, and be driven by a comprehensive set of values such as equity, sustainability, and participation. Ideally they need to be grounded in the Eleven Qualities Hancock and Duhl (1986) outlined, and acknowledge Healthy Cities as a process rather than an intervention. As such, an urban based evaluation of an intervention that aims to reduce the incidence of obesity among children through behavioural change cannot be considered a Healthy City effort; at the same time, a sanitation programme to improve access to safe water recognising the critical role of the local community, women’s groups and good governance may well be a Healthy City (or village) initiative, even when the label ‘Healthy City’ has not been applied.
The effectiveness of the application of principles and values
Healthy Cities are not necessarily interventions – they are value systems and socio-cultural ‘gazes’ that may lead to opportunities for better health and reduction of health inequity. A number of evaluations looked at how such a value system and gaze has come about, and what its influence is on the potential and capacity of the local level to develop novel programmes.
Barton et al. (2013), Baum et al. (2006), Burton (1999), De Leeuw et al. (2014), de Leeuw et al. (2015a, 2015b), Donchin et al. (2006), Hall et al. (2009), Kim (2012), Larsen et al. (2008), Plumer et al. (2010) and Twiss et al. (2000) look at systems-wide and value-based drivers of Healthy Cities. They all find that with careful preparation and conscientious consultation with all stakeholders (including communities and industry, and across government sectors) Healthy Cities create conditions for better governance, enhanced intersectoral action and opportunities for Health in All Policies, and greater resilience of particular programmes when they are facing resource or political turmoil. Lipp, Winters and De Leeuw (2013) in addition find that such a systems perspective creates wider and stronger partnerships for health. Farrington, Faskunger & Mackiewicz (2015) in turn show that enhanced systems parameters, and broader and tighter partnerships secure more effective city-based programmes to facilitate healthier lifestyle choices.
The European Office of the World Health Organization has consistently sponsored and facilitated these types of evaluations of its networks. And consistently they show that taking the time to set the stage in adopting principled values for good governance, community engagement, sustainability and a drive to equity (Ritsatakis, 2009, 2013, Ritsatakis, Ostergren & Webster, 2015) in fact yields results.
Focused interventions from a Healthy City platform
Of course the pointy end of Healthy City initiatives is, and should be, to improve the health of individuals and communities, and to reduce any health inequities. Such an approach boils down to the identification of health threats, disease patterns, and effective interventions. Nam et al. (2011) show that the strong value base of Healthy Cities in the Republic of Korea created opportunities for increased tobacco taxation, the proceeds of these were pumped back into health promotion programmes. The resulting reduction in tobacco consumption is consistent with similar research findings elsewhere, but here we can uniquely attribute the success to the Healthy City vision.
The emerging evidence is strong that embracing general Healthy City values at any level of government or governance yields health and well-being effects, although this evidence as yet is a bit far and wide. Kiyu et al. (2006) evaluate the development and effectiveness of Healthy Villages in Malaysia. A clear and comprehensive vision, engaging the community with respect, leads to sustained outcomes. Nohara et al. (2015) and Mohan, Prathiba &Pradeepa (2014) take a similar approach to diabetes and NCDs in India and find that new IT technologies may enhance and sustain such village-based efforts. Coghlan et al. (2014) look at child wasting in Lao PDR and find sustained health effects of a broad perspective. Fanzo (2014) applies a Healthy Village perspective to matters of food security in the Global South and finds similar results. Masud Rana et al. (2009) investigated quality of life of the elderly in Bangla Deshi villages and support such findings. Even in remote communities in higher income countries this approach works: Tomlin et al. (2012) show that a comprehensive Healthy Village-type programme promotes rural and remote health of children in Canada. Suntayakorn & Rojjanasrirat (2013) demonstrate its effectiveness in the area of stroke reduction in Thailand, and Acharya et al. (2015) in the improvement of maternal and child health in rural India. On the other side of the spectrum, Healthy Communities improve the health and well-being of rural elderly in China, Wang et al. (2014) find.
References
Acharya, A., Lalwani, T., Dutta, R., Rajaratnam, J. K., Ruducha, J., Varkey, L. C., … & Bernson, J. (2015). Evaluating a Large-Scale Community-Based Intervention to Improve Pregnancy and Newborn Health Among the Rural Poor in India. American journal of public health, 105(1), 144-152
Barton, H. & M. Grant (2013) Urban Planning for Healthy Cities: A Review of the Progress of the European Healthy Cities Programme. Journal of Urban Health : Bulletin of the New York Academy of Medicine 90.Suppl 1 (2013): 129-41
Baum, F., Jolley, G., Hicks, R., Saint, K., & Parker, S. (2006). What makes for sustainable Healthy Cities initiatives?—A review of the evidence from Noarlunga, Australia after 18 years. Health Promotion International, 21(4), 259-265
Blum, H. L. (1974) Planning for Health: Development and Application of Social Change Theory. Human Sciences Press, New York
Burton, S. (1999). Evaluation of healthy city projects: Stakeholder analysis of two projects in Bangladesh. Environment and Urbanization, 11(1), 41-52.
Coghlan, B., Toole, M. J., Chanlivong, N., Kounnavong, S., Vongsaiya, K., & Renzaho, A. (2014). The impact on child wasting of a capacity building project implemented by community and district health staff in rural Lao PDR. Asia Pacific journal of clinical nutrition, 23(1), 105
de Leeuw, E., Clavier, C., & Breton, E. (2014). Health policy–why research it and how: health political science. Health Research Policy and Systems, 12(1), 55
de Leeuw, E., Green, G., Spanswick, L., & Palmer, N. (2015b) Policymaking in European healthy cities. Health promotion international, 30(suppl 1), i18-i31
De Leeuw, E., Kickbusch, I., Palmer, N., & Spanswick, L. (2015a) European Healthy Cities come to terms with health network governance. Health promotion international, 30(suppl 1), i32-i44
de Leeuw, E., Tsouros, A. D., Dyakova, M., & Green, G. (2014). Healthy Cities, Promoting health and equity-evidence for local policy and practice. WHO Regional Office for Europe. Copenhagen
Donchin, M., Shemesh, A. A., Horowitz, P., & Daoud, N. (2006). Implementation of the Healthy Cities’ principles and strategies: an evaluation of the Israel Healthy Cities network. Health Promotion International, 21(4), 266-273.
Duhl. L.J., ed. (1963) The Urban Condition – People and Policy in the Metropolis. Basic Books. New York/London
Fanzo, J. (2014). Strengthening the engagement of food and health systems to improve nutrition security: Synthesis and overview of approaches to address malnutrition. Global Food Security, 3(3), 183-192
Farrington, J. L., Faskunger, J., & Mackiewicz, K. (2015). Evaluation of risk factor reduction in a European City Network. Health promotion international, 30(suppl 1), i86-i98.
Goumans, M. J. (1998) Innovations in a fuzzy domain: healthy cities and (health) policy development in the Netherlands and the United Kingdom (Doctoral dissertation, Maastricht University)
Hall, C., Davies, J. K., & Sherriff, N. (2010). Health in the urban environment: a qualitative review of the Brighton and Hove WHO Healthy City Program. Journal of Urban Health, 87(1), 8-28.
Hancock, T. & L. Duhl (1986) Promoting Health in the Urban Context. WHO Healthy Cities Papers No. 1. FADL Publishers, Copenhagen
Kim, J. (2012) Principles of Healthy City Evaluation. 保健 敎 育 · 建康 增進 學會 誌 第 29 卷 4 號, 2012.10, 67-81
Kiyu, A., Steinkuehler, A. A., Hashim, J., Hall, J., Lee, P. F., & Taylor, R. (2006). Evaluation of the healthy village program in Kapit district, Sarawak, Malaysia. Health Promotion International, 21(1), 13-18
Kumaresan, J., Prasad, A., Alwan, A., & Ishikawa, N. (2010) Promoting health equity in cities through evidence-based action. Journal of Urban Health, 87(5), 727-73
Lipp, A., Winters, T., & de Leeuw, E. (2013). Evaluation of partnership working in cities in phase IV of the WHO Healthy Cities Network. Journal of urban health, 90(1), 37-51.
Masud Rana, A.K.M. Wahlin, Å., Stålsby Lundborg, C. & Z. Nahar Kabir (2009) Impact of health education on health-related quality of life among elderly persons: results from a community-based intervention study in rural Bangladesh. Health Promotion International, 24 (1) 36-45
Mohan, V., Prathiba, V., & Pradeepa, R. (2014). Tele-diabetology to Screen for Diabetes and Associated Complications in Rural India The Chunampet Rural Diabetes Prevention Project Model. Journal of diabetes science and technology, 8(2), 256-261
Moysés, S. J., Moysés, S. T., McCarthy, M., & Sheiham, A. (2006). Intra-urban differentials in child dental trauma in relation to healthy cities policies in Curitiba, Brazil. Health & place, 12(1), 48-64
Nam, E. W., De Leuw, E., Moon, J. Y., Nayu, I., Dorjsuren, B., & Park, M. B. (2011). Sustainable funding of health initiatives in Wonju, Republic of Korea via a tobacco consumptio
Nohara, Y., Kai, E., Ghosh, P. P., Islam, R., Ahmed, A., Kuroda, M., … & Nakashima, N. (2015). Health Checkup and Telemedical Intervention Program for Preventive Medicine in Developing Countries: Verification Study. Journal of medical Internet research, 17(1)
Plümer, K. D., Kennedy, L., & Trojan, A. (2010). Evaluating the implementation of the WHO Healthy Cities Programme across Germany (1999–2002). Health promotion international, daq028. 342-54
Ritsatakis, A. (2009). Equity and social determinants of health at a city level. Health promotion international, 24(suppl 1), i81-i90
Ritsatakis, A. (2013). Equity and the social determinants of health in European cities. Journal of Urban Health, 90(1), 92-104
Ritsatakis, A., Ostergren, P. O., & Webster, P. (2015). Tackling the social determinants of inequalities in health during Phase V of the Healthy Cities Project in Europe. Health promotion international, 30(suppl 1), i45-i53
Suntayakorn, C., & Rojjanasrirat, W. (2013). Effects of an empowerment program on health behaviors and stroke risk reduction of at-risk group in Thai rural community. Journal of the Medical Association of Thailand= Chotmaihet thangphaet, 96(9), 1229-1238
Takano, T. (Ed.). (2003). Healthy cities and urban policy research. Routledge
Tomlin, D., Naylor, P. J., McKay, H., Zorzi, A., Mitchell, M., & Panagiotopoulos, C. (2012). The impact of Action Schools! BC on the health of Aboriginal children and youth living in rural and remote communities in British Columbia. International journal of circumpolar health, 71.
Twiss, J. M., Duma, S., Look, V., Shaffer, G. S., & Watkins, A. C. (2000). Twelve years and counting: California’s experience with a statewide Healthy Cities and Community program. Public health reports, 115(2-3), 125
Wang, J., Chen, C. Y., Lai, L. J., Chen, M. L., & Chen, M. Y. (2014). The effectiveness of a community-based health promotion program for rural elders: A quasi-experimental design. Applied Nursing Research, 27(3), 181-185






